Monica Bodd thinks a lot about the patient experience and how to make it better — both through research and clinical practice.
While earning her MD and her Masters of Theological Studies degrees at Duke, she learned from some of the best, including Thomas LeBlanc, MD, MA, MHS, Dan Rocke, MD, JD, and Walter Lee, MD, MHS, from Duke Cancer Institute, and from the Duke Divinity School, Warren Kinghorn MD, ThD, Sarah Barton OT, ThD, Susan Eastman, MDiv, PhD, and Kate Bowler, PhD.
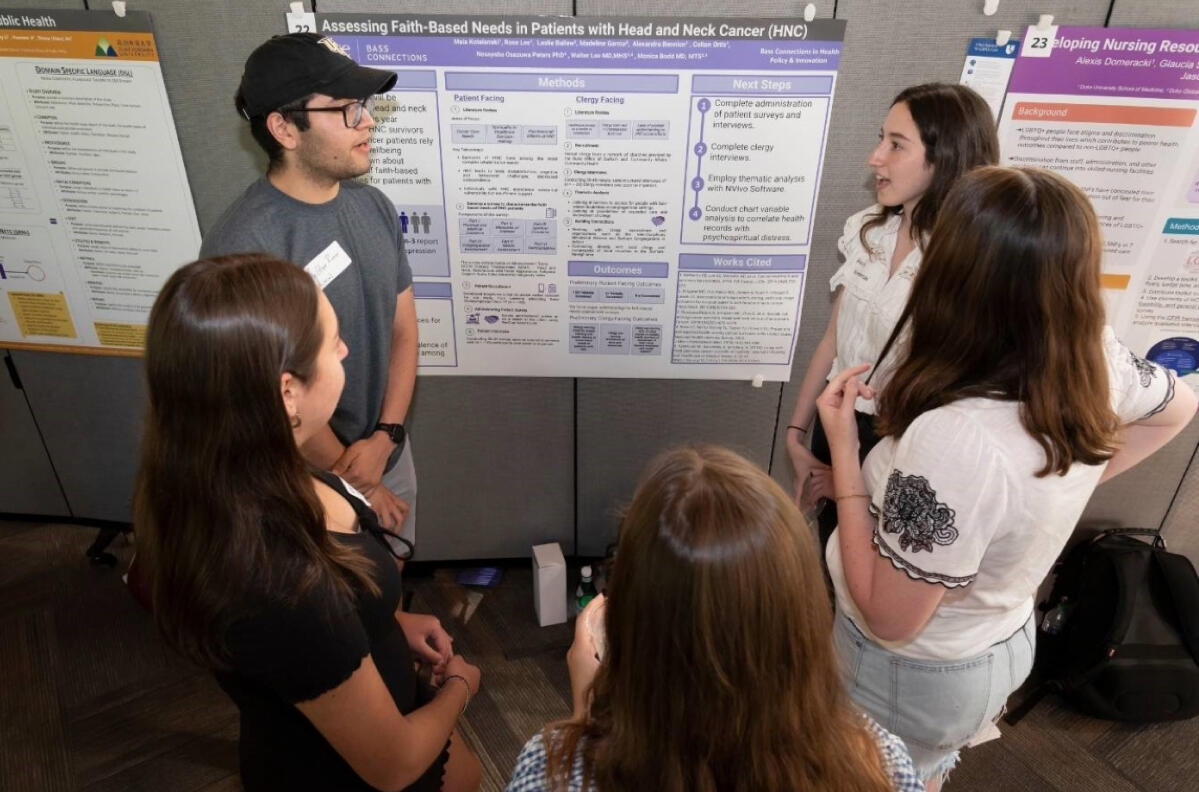
Patient experience research in oncology is an investigation of common issues faced by people with cancer, including symptom burden, quality of life, and psychological distress, as well as how patients understand their prognosis and make decisions about their treatment through the various stages of their disease.
“The way I explain it to my friends or to my family, it’s about asking patients how they live and work through their diagnoses on a day-to-day basis, centering their perspective over the perspective of a medical record or a diagnosis or a doctor's words,” said Bodd. “There are validated and quantitative aspects to it, but it’s more about what we wouldn't necessarily capture with our big data and metrics… I believe it’s the redeeming hope for a lot of medicine.”
As Bodd was leaving Duke to begin her residency in Otolaryngology-Head & Neck Surgery at Stanford Medicine this past spring, she spoke with DCI about some of the unique projects she got to work on and co-lead as a medical student and theology student — and the wisdom and practices she’s carrying forward in her medical career from both disciplines.