For decades, bone marrow transplantation has saved the lives of patients with blood cancers or other inherited or acquired bone marrow diseases. But today, it’s helping more people than ever because medical advances have made the procedure feasible for more patients.
Bone marrow is spongy tissue in our bones that houses the blood stem cells that give rise to red blood cells, platelets, and the workhorses of the immune system, white blood cells. In a bone marrow transplant, stem cells from healthy bone marrow or blood are infused into a patient to do the work of producing blood cells. Patients with certain blood cancers like lymphoma may need a transplant if the chemo or radiation necessary to kill their cancer also kills their bone marrow. In other cases, the recipient’s bone marrow stem cells may be producing blood cells, but those cells aren’t up to the task of recognizing and killing cancer and need to be replaced with stem cells from a healthy donor.
The transplanted cells can come from the patient (collected ahead of time) or from a donor. In the past, patients in need of a transplant had to have a matched donor, meaning that recipient and donor had the same immunologic proteins, called HLA. Otherwise, the donor cells would launch an immune attack on the recipient’s body.
Over the last few decades, researchers have made significant progress in discovering how to perform transplants using donated cells that aren’t a perfect match. Furthermore, stem cells can now be harvested not just from bone marrow but from blood and umbilical cord.
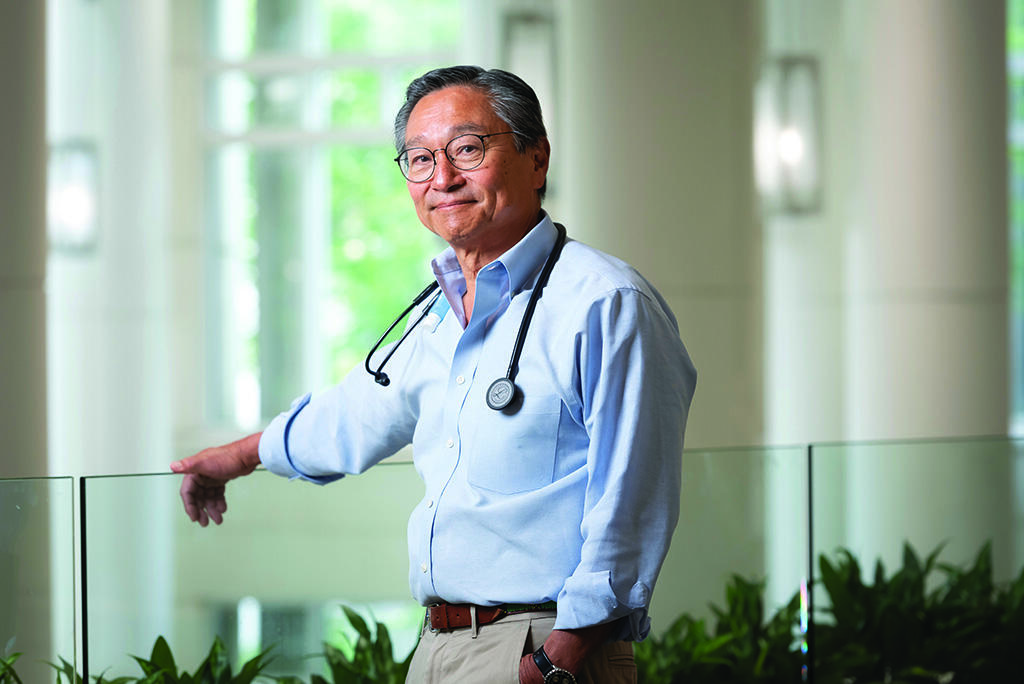
“More patients can benefit from transplantation now because there are more donor options,” said Edwin Alyea, MD, the chief medical officer of the Duke Cancer Institute. “And we can now offer reduced intensity transplants, with lower-dose chemotherapy, to patients who were previously not eligible because of age or other medical problems.”