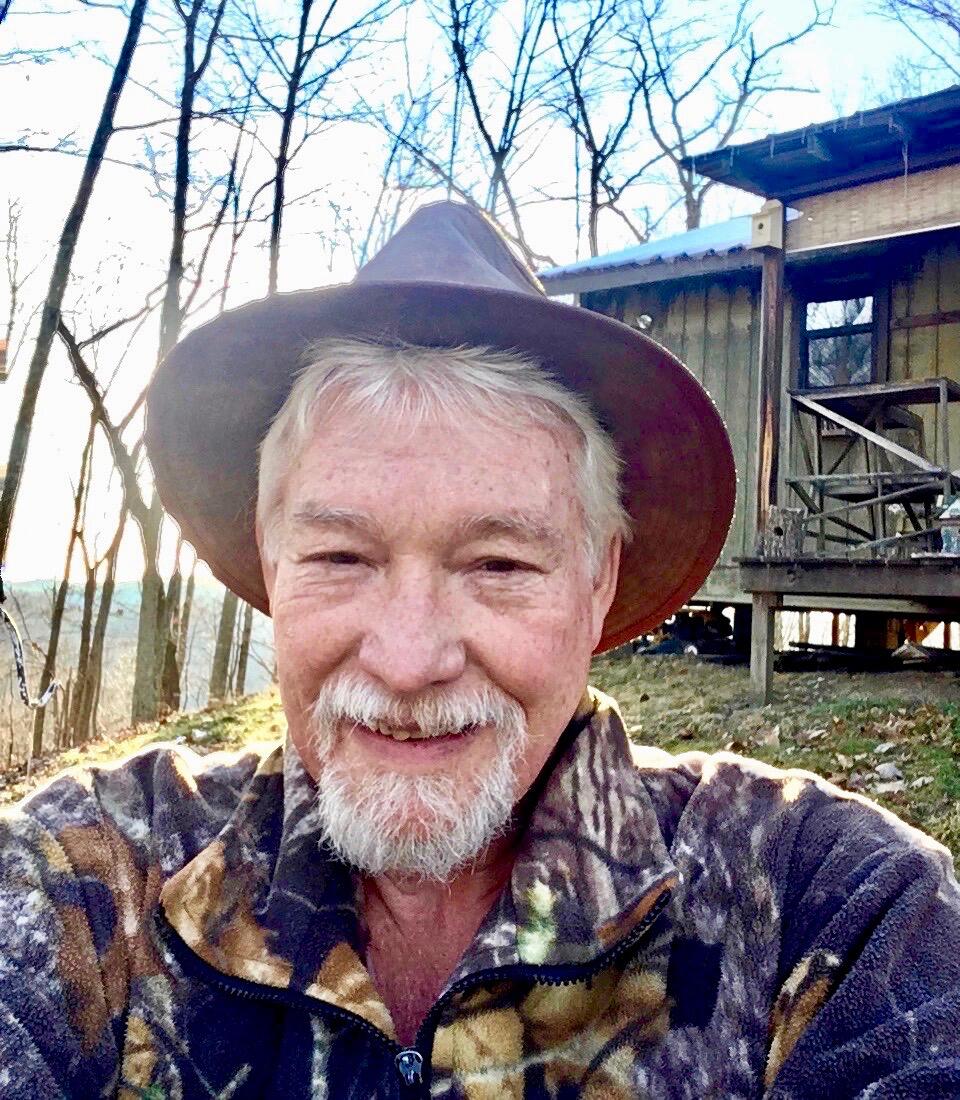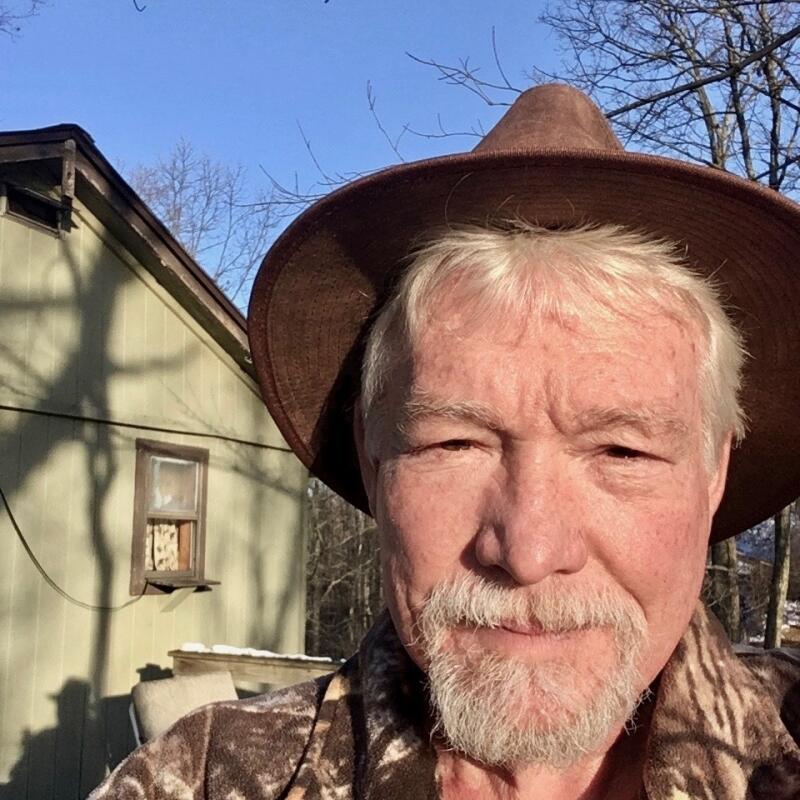
William Blake, 65, worked for the State of West Virginia for about 35 years in the toll division before taking early retirement in 2007 when he got sick with follicular lymphoma. He was treated at Charleston Area Medical Center (WV) and survived that cancer.
But when Blake was diagnosed four years later with a different type of cancer at the Beckley, WV, Veterans Hospital — metastatic melanoma to the brain — he was referred to Duke.
John Kirkpatrick, MD, PhD, the director of radiation oncology for The Duke Center for Brain and Spine Metastasis at Duke Cancer Institute and clinical director of radiation oncology at DCI, performed an image-guided stereotactic radiosurgery (SRS) procedure on Blake’s two brain lesions — a high-tech non-surgical therapy that delivers precisely-targeted high-dose radiation in one to five treatments, while preserving nearby healthy tissue.
Medical oncologist April Salama, MD, meanwhile, treated Blake with a course of ipilimumab, an immunotherapy that had just been approved that year for the treatment of advanced melanoma. When another lesion appeared in March 2012, Kirkpatrick “disappeared” that one as well.
“The prognosis was “We’ll do what we can, the mets are really small, and we caught it early,”” said Blake, who’s today making the most of his retirement.
While Blake has recently had some small localized melanomas and basal cell carcinomas removed in other areas of his body, there’s been no sign of cancer in his brain for seven years.