During the summer of 2016 Dave and Lisa VanTress retired from their jobs in Syracuse, New York, and headed south to the sunny shores of South Carolina, where they could be close to family and indulge their passion for fishing. They bought a townhouse in Little River, a five-minute drive to the beach.
Around Mother’s Day weekend the following year, Dave and Lisa, the parents of six grown children, embarked on a 12-hour fishing charter. Three hours motoring out to sea. Six hours fishing. And three hours back. They caught a lot of fish that day.
“It was a great trip, but when I got off the boat, I couldn’t regain my ‘land legs,’” said Lisa VanTress, then 55 years old. “I was unstable on my feet. For the next couple days, I was stumbling around and I even fell down the stairs.”
She was treated for suspected seasonal allergies. But within a week-and-a-half, she took a nasty tumble while getting into bed. A trip to the emergency department (ED) revealed, by her description, “two huge cancerous brain tumors.” Further investigation indicated, to her surprise, that she had lung cancer.
Nearly 150,000 Americans annually are diagnosed with cancer that has metastasized, or traveled, to the brain. The number is projected to rise. Because of a larger aging population, combined with improvements in cancer screening and care, up to 30 percent of patients with solid tumor cancers (mainly lung cancer, breast cancer, melanoma, genitourinary cancers, and renal cell carcinoma) can expect their cancer to spread to the brain.
Duke Cancer Institute (DCI) is addressing the needs of these patients head-on. This past fall, DCI, in collaboration with the Department of Neurosurgery and the Translating Duke Health Initiative, launched the Duke Center for Brain and Spine Metastasis at Duke Cancer Institute — an outgrowth of the Duke Brain Metastasis Program.
Co-directing the new multi-disciplinary center are neurosurgeon Peter Fecci, MD, PhD, breast oncologist Kimberly Blackwell, MD, and radiation oncologist John Kirkpatrick, MD, PhD.
Surgeons, oncologists, and radiation oncologists affiliated with the center are nationally known for their use of cutting-edge technologies that prolong life, and the center is actively both participating in and sponsoring groundbreaking research to better understand brain and spine metastasis and develop new treatments.
"Brain metastasis used to be viewed as a death sentence and patients were rarely even offered surgical treatment, but as the quality of our treatments has improved, so has survival,” said Fecci, who launched the Duke Brain Metastasis Program shortly after he arrived at Duke in 2014. “Some of my first patients are still alive and doing well, while a decade ago that type of survival was just a dream.”
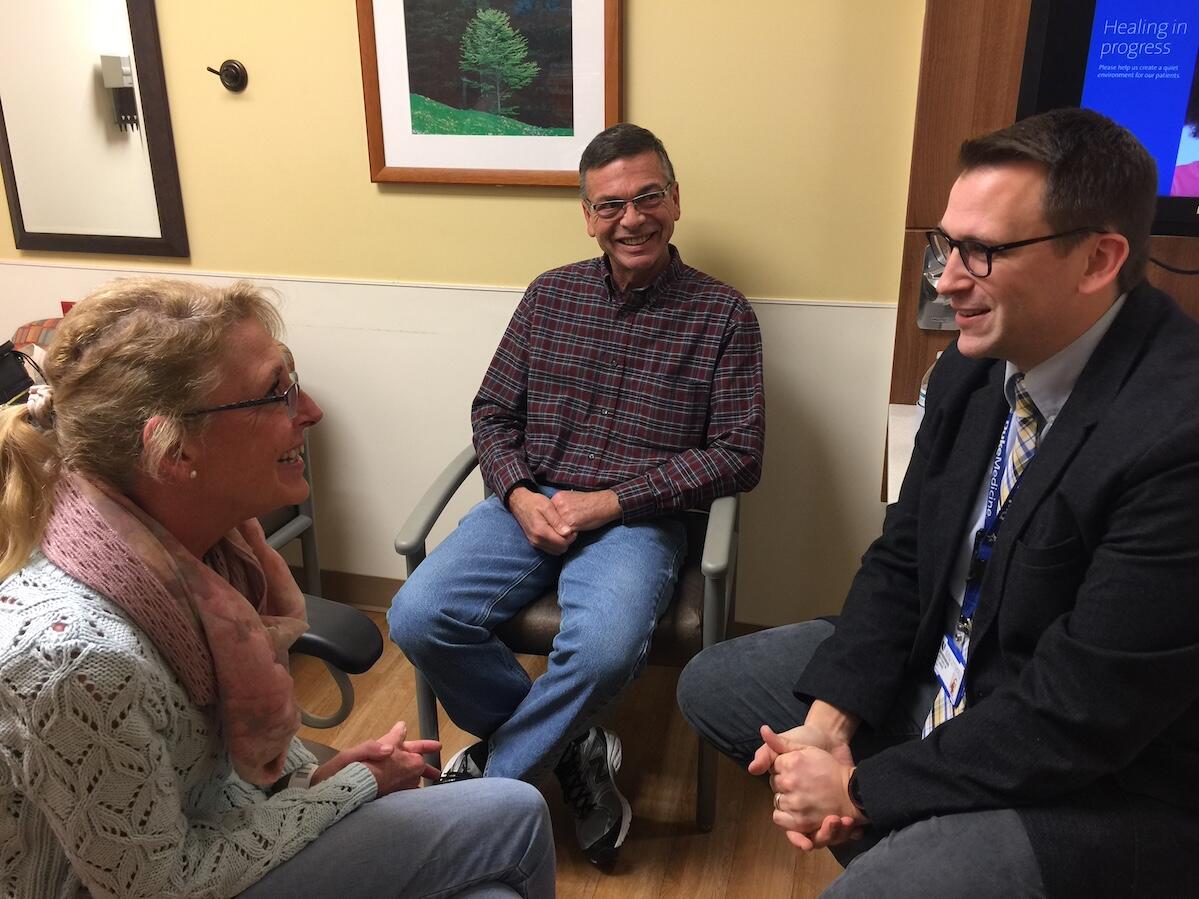
VanTress eventually found her way to Fecci’s operating room — a three-hour drive from home — after initially being told by her local oncologist she should fly her family in and get her affairs in order because there was nothing more to be done. And, so, she did, anticipating the end was near. However, her eldest brother, a hospital CEO in a neighboring county, quickly made some phone calls and connected her with Duke for a second opinion.