Pancreatic cancer is one of the most challenging types because it is most often diagnosed in the late stages, when surgery isn’t possible. In 2022, the five-year survival rate for the disease is 11%, a slight increase from last year, according to the American Cancer Society.
To make outcomes better, researchers around the world are trying to find a marker from blood or some other bodily fluid that would reliably diagnose pancreatic cancer in its early stages, said Jim Abbruzzese, MD, Duke Cancer Institute Distinguished Professor of Medical Oncology. Abbruzzese sees promise in a test that has been studied in the lab of Chris Counter, PhD, George Barth Geller Distinguished Professor of Pharmacology. Abbruzzese and hematology/oncology fellow Ryne Ramaker, MD, PhD, are beginning work to translate it to patients.
Counter’s lab tries to capture the moment when a normal cell progresses to a tumor, then study it. Even in a cancer with lots of successful treatment options, like melanoma, the best bet is still finding the disease early, said Counter, whose mother-in-law Linda Woolfenden died of melanoma. It’s even more important in a challenging disease like pancreatic cancer.
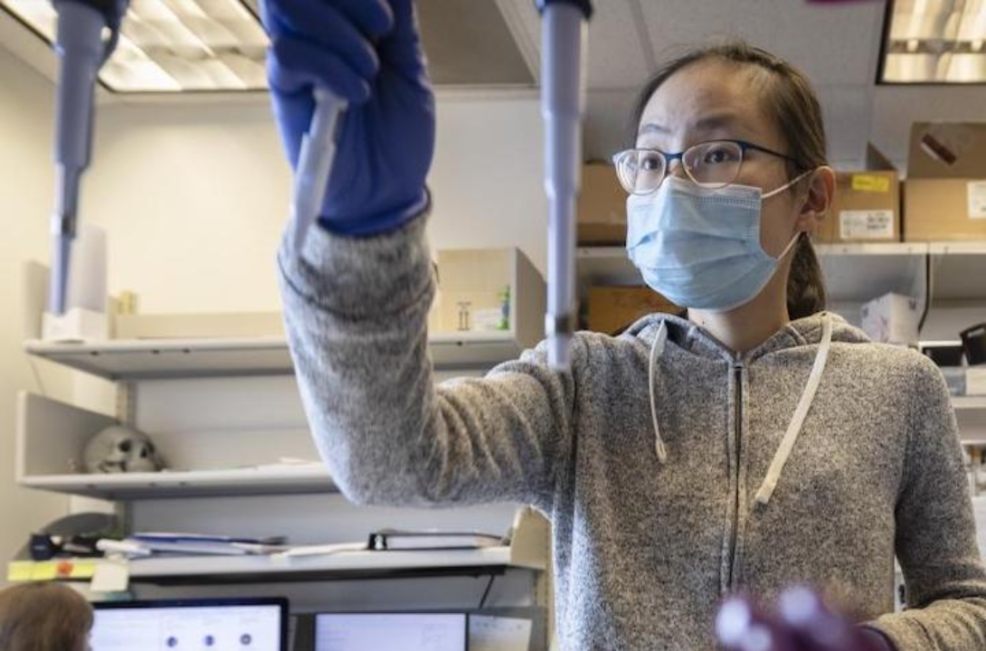
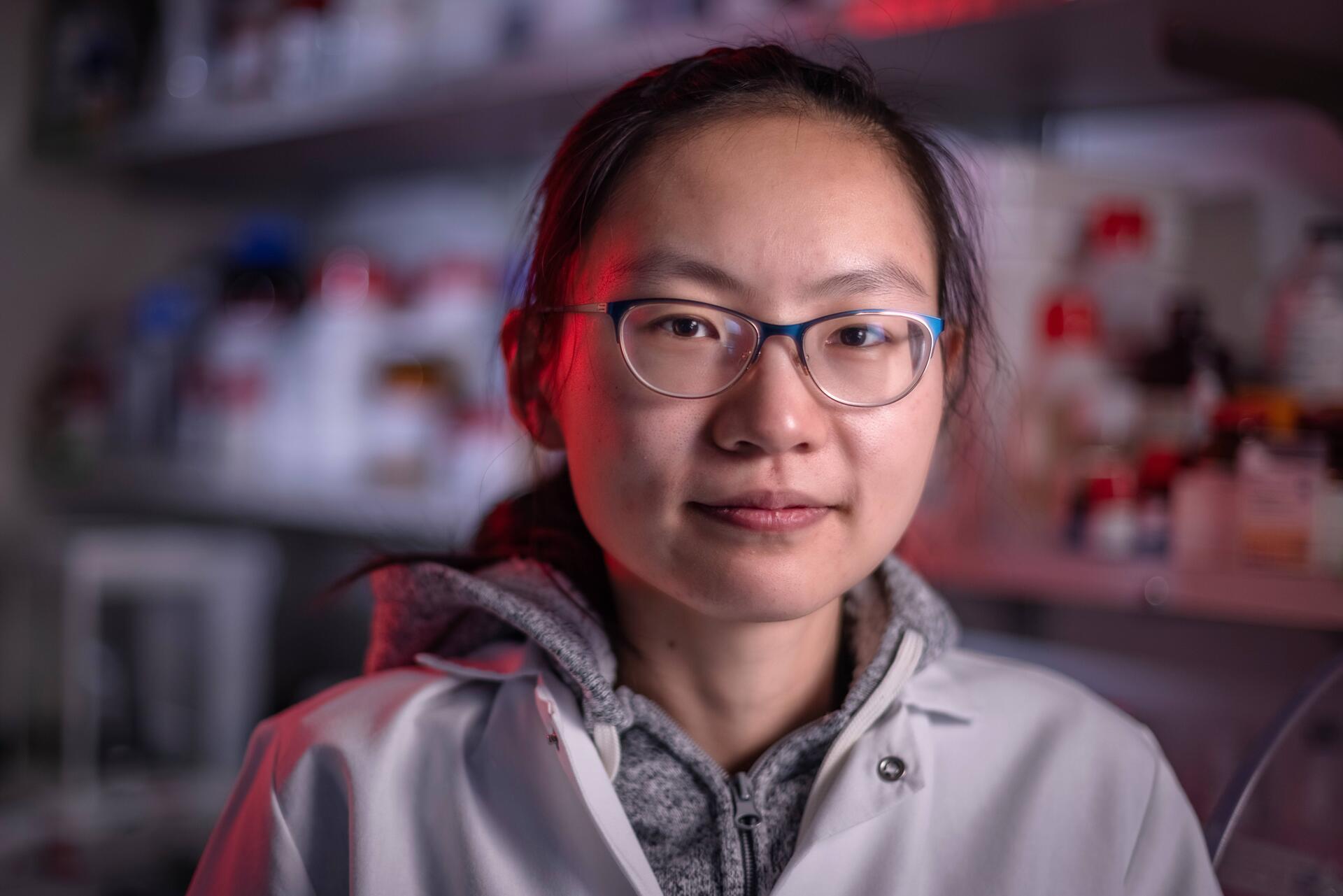
Siqi Li, PhD, now a Damon Runyan fellow at Fred Hutchinson Cancer Research Center, was a PhD student in Counter’s lab when she became intrigued by a method called maximum-depth sequencing, which was developed by researchers in the lab of Evgeny Nudler, PhD, at New York University to detect mutations that lead to antibiotic resistance in bacteria.
“Siqi saw the parallels between bacteria and cancer, and she was very interested in using this assay in mammals,” Counter said. “So she adapted this assay with the help of the lab of Dr. David McAlpine here at Duke for the mammalian genome to capture mutations causing cancer.”
Counter’s team found that this technology captures mutations that are too few and far between to be detected by traditional next-generation gene sequencing. “The assay was so sensitive, that Siqi was able to detect a cancer-causing mutation a week after mice were exposed to an environmental carcinogen,” Counter said. The team published results of this work in 2020 in the journal Nature Communications and in 2022 in the journal eLife. The studies were supported in part by a Duke Cancer Institute pilot grant, a program sustained by donor funds.
The test holds promise not only because of its sensitivity, but also because it’s specific to KRAS, a gene commonly mutated in pancreatic cancer, Abruzzese said.