Janel Keaton has been able to travel for weddings and grandbabies and to enjoy mountain hikes and coastal cycling as a stage 4 breast cancer patient, thanks, in part, to the expert care team at the Duke Center for Brain and Spine Metastasis who have her back — from nurse navigation to interventional radiology, pain management, palliative care, radiation oncology, and medical oncology.

They've Got Her Back
Published
 From the Duke Cancer Institute archives. Content may be out of date.
From the Duke Cancer Institute archives. Content may be out of date.

LAST SUMMER, Janel and Troy Keaton were blessed with two grandbabies — their fifth and sixth — born within four days of each other to their daughters Natalie and Allyson. In August, the couple attended their son Trevor’s wedding. And in late February, they attended their other son TJ’s wedding.
“Having a metastatic cancer diagnosis means: The future is something you wonder about,” wrote Janel on her Facebook page a few days after that last wedding. “When you find out about expectant births or weddings you always wonder if you will ‘make it till then’... I was there for all of them! I am so thankful. God has been good to us!”
Troy grew up in Indiana and Janel Keaton’s from Pennsylvania. While they began their married life in Tennessee in 1999, the couple felt called to settle in the Smith Mountain Lake area of the Blue Ridge Mountains in Virginia.
That's where Troy, with 60 parishioners, first “planted” the non-denominational EastLake Community Church 16 years ago, and where now, as senior pastor, he ministers to more than 1,500.
Janel is not on staff at the church. She never wanted a visible role there. While Troy is gregarious and popular, Janel is the quiet, no-drama low-maintenance type. So, when their kids started a Facebook page right after Janel’s stage 4 breast cancer diagnosis to keep friends, loved ones, and the wider church community updated, they didn’t imagine that she’d be an active participant.
Just two weeks later, however, Janel taped a video message for her followers.
“We hate everything about this diagnosis, but I'm not curled up in a fetal position in the corner of the couch crying my eyes out, although I probably have done that once or twice,” she shared, in her first video post. “This is not fun to have to navigate life in a different way and know that it will never be the same again. Medically, this is not good. This is a terminal diagnosis. And I know that ... I'm not stomping my feet and holding my breath expecting God to perform a miracle for me. I'm praying for it, and I hope you are too, but I trust my Father in Heaven to do what is best.”
She thanked everyone for loving, supporting, and praying for them — “the oil to our gears and water to our souls” — and she reassured them that she’d been granted the gift of “absolute peace” in her heart by God with her new reality. Her authentic posts have continued, and many thousands have responded.

In God’s Hands, In Good Hands
“We believe very strongly that bad things happen to everybody and good can come out of it if you allow God to work, and she's really committed to that; even sending notes and messages to people in difficult situations,” shares Troy during an interview with the couple in February. “Janel is a great blessing now to a lot of people, more publicly than she's been before. She’s gotten more spotlight on her than she ever wanted. At church they used to line up to talk to me, and now they line up to talk to her.”
“People always get cancer, but it's always somebody else, you know,” adds Janel. “And it’s really been a weird thing that ‘oh my word this is our life now.’ I think cancer sucks. I hate it. I hate it. I would get rid of it in a heartbeat if I could, obviously, but I know that good will come out of it.”
“It,” unbeknownst to Janel, had all started in 2019, when she first felt what she described as “a kind of long lump” in her breast.
She had no family history of breast cancer and after assurances from a doctor that the mass was typical and typically benign in pre-menopausal women, Janel (then 51) assumed it was indeed that — just her age catching up with her. She continued to maintain her active lifestyle, only realizing later that cancer had been growing in her body for some time.
In 2020 sudden pain from what she assumed was a broken rib sent Janel back to the doctor. This time, a mammogram and an x-ray were ordered. The x-ray, the doctor reported, looked fine. The mammogram, however, was suspicious for breast cancer. Since it appeared to be confined to a small tumor, she told Janel not to worry and scheduled her to have the mass surgically removed the following week.
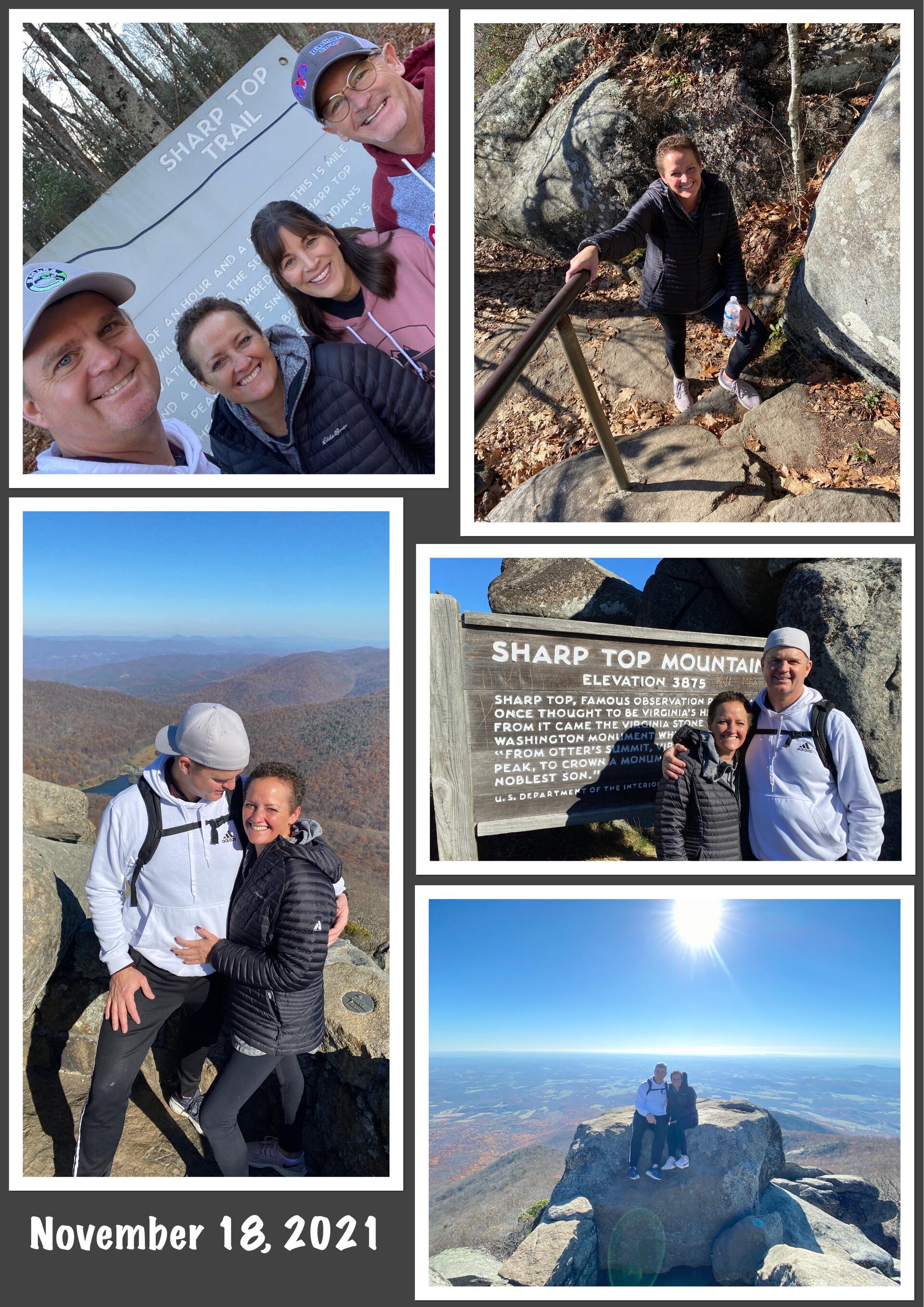
But during that week before surgery, Janel’s back began randomly locking up; immobilizing her leg for brief periods. One day that week — on November 18, 2020 — the pain was so severe she couldn’t make it off the couch. She called Troy, who was quarantined with Covid, for help. Troy called the surgeon who requested Janel come immediately for a CT scan. The CT revealed cancer in her ribs, spine, and possibly her ovaries. Stage 4. Because it had already spread beyond the breast, surgery to remove her breast tumor was cancelled.
The couple asked around and found “a great oncologist with a great reputation” with whom to pursue next steps about 20 minutes down the road in Roanoke — Andrew Fintel, MD, at Blue Ridge Cancer Center.
After a couple weeks, with her life in the balance, friends recommended they pursue a second opinion from a research facility. Troy called the University of Virginia Medical Center, but the friend of a friend who worked there diverted him to Duke for their expertise in treating breast cancer.
“We were able to get into Duke within a week of our request,” said Troy. “We were amazed by the level of care.”
It Takes a Village
The Duke Center for Brain and Spine Metastasis (DCBSM) – where Janel was referred — is one of Duke’s fastest-growing clinical programs. Launched in 2017 by Duke Cancer Institute in collaboration with the Department of Neurosurgery and Translating Duke Health (a 5-year initiative of Duke University Chancellor for Health Affairs Eugene Washington, MD, MPH, MSc), the Center has become one of the most comprehensive destination programs in the country for treating this growing population of patients.
Continuously building on the strong collaboration between the Department of Neurosurgery, the Department of Radiation Oncology, the divisions of Medical Oncology and Palliative Care, and the Neuro-Oncology program, the DCBSM boasts more than 50 clinical specialists.
This includes nurse navigators, nurses, physician assistants, medical oncologists, radiation oncologists, neurosurgeons, palliative care and pain management specialists, as well as neuroplastic surgeons, neuroradiologists, interventional radiologists, spine experts, and physiatrists.
The Center has navigated more than 2,000 patients to care since the Center launched.
Patients whose cancer has spread to the brain, spine, or other areas of the central nervous system require highly specialized and incredibly complex care. Navigation sets the tone for their experience.
“What I think the newly diagnosed need most is somebody to say, ‘I understand you're scared. I would be too. This is what we do all day, every day, and we're going to create a plan for you. And as long as you want us, we're going to walk this journey with you.’ And then they just kind of breathe out... And then we can build a fantastic team around their particular needs,” explains DCBSM nurse navigator Scott Pollard MSW, BSN, RN — a nurse with oncology and Neuro-ICU bedside and clinical research experience and a former social worker skilled in short-term crisis management, listening and reflection, and other supportive care strategies. “It's nice to feel confident in your team, knowing they're top of the game.”

The Center’s promise to its patients is access to navigated care, embedded palliative care, and an inpatient consultation service; access to genomic testing, the latest therapies, and cutting-edge clinical trials; and review of their case by a multi-disciplinary team of DCBSM specialists.
Once a patient’s care team is assembled the team works with the patient to define goals of care and to forge the best treatment path forward.
“To reduce stress for patients, we arrange for them to see all needed providers within 72 hours — all under one roof,” explains DCBSM program manager Natalie Ashley, BN, GradDipAdvn, who was recruited to the DCBSM in early 2018 as the Center’s sole patient navigator/new patient coordinator and named program manager in January 2020.
Ashley drew on her experience in Australia as a nurse navigator to help grow the patient navigation team from a team of one (just herself) to a team of three including a new-patient coordinator (Eris Worlds) and two nurse navigators — one for spine mets patients (Pollard), brought on in January 2020, and one for brain mets (Donie Magee, RN, BSN, CHPN), brought on in March 2020.
“Our navigation team understands the daily needs of our patients and their loved ones and how to guide them through the complex cancer care system — from addressing barriers to access, to educating them about planned and potential treatments, to providing emotional support. They bring together all the moving pieces of a patient’s care plan and bridge any gaps throughout their cancer journey,” continues Ashley.

Carey Anders, MD, a nationally recognized specialist in breast cancer that has spread to the central nervous system, took the lead on Janel’s case.
“Janel was very symptomatic and on a rocky course when I first saw her in clinic. In the first meeting with a patient, we think in terms of weeks, months and years. In Janel’s case, I said, ‘We're aiming for years with you,’” recalls Anders, a Translating Duke Health Scholar and medical director of the DCBSM since early 2019.
Janel’s cancer is triple positive — ER+ (estrogen receptor positive), PR+ (progesterone receptor positive) and HER2+ (human epidermal growth factor receptor 2 positive). Fortunately, there are many therapy options for this type and stage including HER2- targeted therapies, endocrine (hormone-blocking) therapies, chemotherapies, and aromatase inhibitors; all of which cut off the fuel that contributes to cancer growth.
Her type of breast cancer was initially thought to be HER2 negative (following biopsy in November 2020), but after subsequent confirmatory testing of the subtype, it turned out to be HER2 positive (amplified), which, as Anders explained, broadened the treatment possibilities.
Anders worked with Janel’s local oncologist Andrew Fintel, MD, to quickly switch course. Once Anders and Fintel decided on a new drug formulation, Janel was able to continue her infusion treatments and oral drugs in Roanoke, and with one modification, remains on that regimen today.
Every three months, Anders reviews Janel’s scans and communicates the results and her recommendations back to Andrew Fintel, MD.
“We talk on the phone or via email about Janel’s care. It’s a really nice relationship,” says Anders, who also treats patients in South Carolina, Texas, Mississippi, and all over the U.S., in partnership with their referring physicians. “One of the things that we've really tried to advocate for at the DCBSM is maintaining that relationship with the patient and their referring provider. This works well for folks who don't live right near Duke, and it also allows us to still have a touchpoint with them every three months or so for their restaging, treatment decisions, and next steps.”
When patients need access to more specialized or technologically advanced procedures, surgeries, scans, and genomic testing they can’t get locally, as well as DCBSM-grown and national DCI-site clinical trials, they can travel to Duke.
This is the case with Janel, who has at least four other DCBSM specialists on her care team — providers who’ve deployed treatments and procedures to ease her pain, improve mobility, and control her cancer.
Associate Radiation Director of the DCBSM, Scott Floyd, MD, PhD, joined Janel’s care team almost immediately.
“Her tumors were quite extensive when we met her,” says Floyd, who, beginning in December 2020, administered a five-day course of conventional radiation therapy to treat several spots where her breast cancer had spread, including bone tumors in her pelvis, lower back, and left ribs.
“This ‘conventional radiotherapy’ approach, covering larger areas with large radiation fields at modest doses, allows us to help with pain in these multiple sites with lower side effects and to get through the course of treatment in five days,” explains Floyd. “This type of radiation will often shrink the tumors and also helps with pain as tumors pressing on bone and nerves can be very painful.”
In May 2021, Janel underwent another five-day course of conventional radiation therapy — this time to treat metastases in the thoracic and high-lumbar areas of her spine.

That same month — with large tumors bearing down on two of Janel’s vertebrae, one of which had already caused a compression fracture — Janel was assessed by physician assistant Brice Painter, PA-C, MHS (assistant program manager of the DCBSM) in the spine metastasis clinic.
Painter, who works with spine surgeon Rory Goodwin, MD, PhD (surgical director of the DCBSM) referred Janel to DCBSM anesthesiologist and pain medicine specialist Tom Hopkins, MD, MBA, who proposed an additional strategy to keep Janel moving. Hopkins performed a minimally invasive, same-day surgical procedure that included radiofrequency ablation, vertebral augmentation (kyphoplasty), and a biopsy. This all-in-one approach — to further ease Janel’s pain, slow tumor growth, and strengthen and stabilize her spine — doesn’t require general anesthesia and involves minimal recovery time.
Radiofrequency ablation — the delivery of radiofrequency waves directly into the tumor and surrounding tissue via a probe — is used to shrink the tumor, causing tumor cells to die, and may also help to reduce patients' pain.“As the heat destroys the tumor cells, the immune system removes them from the body and the tumor shrinks,” Hopkins explains, adding that cryotherapy (applying extremely cold temperatures to the tumor through the probe) can do much the same thing.
Kyphoplasty — applying cement to the bone — helps stabilize current fractures, prevents future fracturing, and relieves pain. Since bones with tumors are weaker and very susceptible to fractures, both of Janel’s vertebrae (the one with a fracture and the one without) were treated this way.
“Pain relief after a kyphoplasty is typically immediate. Patients wake up feeling better, which allows them to get back to their normal routine that much quicker and, with less risk of fracture, patients feel more at ease and it’s safer for them to get back to the kind of physical activities they enjoy, like in Janel’s case hiking and cycling,” says Painter.
No Crystal Ball

As of May 2022, Janel’s still responding well to treatment.
Floyd notes that the combination of conventional radiation therapy, conventional chemotherapy, targeted therapy, cryotherapy, and sometimes surgery and radiofrequency ablation “can control tumor growth in the bones and spine for long periods of time.”
Anders says that should Janel’s cancer develop resistance to her current cancer meds there are “very clear data ... on very good therapies in the HER2-positive space” that she can try next.
Janel’s cancer, like all cancers, has its own genomic profile that Anders measured early on by testing the tumor DNA circulating in her blood.
“The nice thing is that we have a baseline and if we see changes in the future with her cancer, I can test her blood again and see what resistance mechanisms may have emerged that we can treat — either with a known therapy or a therapy being tested in clinical trials,” says Anders. “We never know when things may change, we're never given that crystal ball.”
Janel, through all this, has learned to be an advocate for her health, including asking questions if there’s something she and Troy don’t understand and not stopping until they get answers. Their “scanxiety” is real.
“Troy’s comfortable calling in and asking questions, which I'm glad of, I wish they all were,” says Pollard, who’s walked the cancer path with Janel and Troy for more than a year now. “I tell my patients, ‘If you are nauseous, call me. If you are afraid that something is being missed, call me. If you don’t know what to expect during a procedure, call me. If you need a referral for counseling, call me.’ Patients don’t schedule appointments with me, and I don't even have a calendar, but I'm certainly a pair of ears and if they need to talk, I will listen.”
Betsy Fricklas, PA-C, MMSc, one of two palliative care specialists embedded within the DCBSM, has also been with Janel since the beginning, helping manage, with medication, Janel’s cancer-related pain that’s not eased in other ways as well as the gastrointestinal and other physical side-effects of cancer treatment. "Palliative care provides relief from the symptoms and stress associated with serious illness, with the goal of improving quality of life for both the patient and their loved ones,” says Fricklas, who joined the DCBSM’s palliative care clinic on November 30, 2018. “I focus on helping people live as well as possible."
Whatever their patients’ care goals, the DCBSM care team has their back every step of the way.
Reflects Pollard, “Cancer patients amaze me with the strength and the reserves they develop. A lot of our patients die. And I know that. I've worked with many who come in saying, ‘I want to fight.’ ‘Okay,’ we say, ‘We're gonna fight with you, let's do this.’ And then at some point, when it's not working, they say, ‘You know, I'm just so tired, I can’t do this anymore, but we fought the good fight.’ And we know we helped them fight their best fight, took on cancer on their terms and relented on their terms. Cancer’s a beast. We hope for the best, but it doesn't always happen. But something is always learned and what we learned will help somebody else.”
Shares Janel, “I have stage four cancer, and I know what that means. But I also have a lot of life left in me and I have a lot to live for. We want to make this (my life) last as long as possible and with as good a quality of life as possible. So that's why we sought out the best treatment. Ultimately, it's in God's hands. He decides, but I do believe that he gives wisdom to doctors, the best doctors, we believe in that. We believe in medicine. We feel very blessed to be patients of Duke. We feel very secure in their hands.”
You can follow Janel on social media on Facebook @Janelkeatonsjourney and/or on Instagram @janel_journey
Follow the Duke Center for Brain & Spine Metastasis on Twitter @DukeMets

Janel's cancer story was updated and adapted in August 2022 for a Duke University School of Medicine series of articles exploring how Translating Duke Health has changed the healthcare landscape at Duke.



