The grants, made possible by the Susan G. Komen Metastatic Breast Cancer Collaborative Research Initiative, have been awarded to teams comprised of patient advocates and DCI and UNC Lineberger Comprehensive Cancer Center investigators.
National breast cancer organization Susan G. Komen announced, on Sept. 13, the awarding of $1.5 million total for three new metastatic breast cancer research projects — each co-led by a Duke Cancer Institute investigator and a UNC Linberger Comprehensive Cancer Center investigator.
These particular grant awards — $500,000 each over three years for each project — will boost evidence-based research into the biological and societal drivers of breast cancer metastasis and mortality and will catalyze the development of potential new treatments.
The grants have been made possible by the Susan G. Komen Metastatic Breast Cancer Collaborative Research Initiative, an innovative, first-of-its-kind collaboration between the Susan G. Komen organization, Duke Cancer Institute, and UNC Lineberger Comprehensive Cancer Center. Pam Kohl, who spearheaded the initiative and serves as its development director, is a metastatic breast cancer thriver being treated at Duke Cancer Institute.
“Research is HOPE for the far too many of us who are living with MBC," said Kohl in a press release from Komen. "This disease is smart, and it is relentless, but I know that these brilliant researchers at UNC and Duke will work every day to help give us the gift of time.”
All three project teams include researchers as well as cancer patient advocates who have a personal stake in this fight.
Breast cancer that has metastasized — most commonly to the bones, liver, lungs or brain — has a 5-year relative survival rate of only 29%. Metastatic breast cancer kills more than 44,000 people in the U.S. every year.
"I am confident that when patients and researchers come together as one that the needle will begin to move on metastatic breast cancer and make a life and death difference in the lives of those like me," said 10-year MBC survivor Katrina Cooke, a patient advocate with Komen North Carolina Triangle to the Coast and member of the Duke Cancer Institute Oncology Patient and Family Advisory Council who's also on one of the DCI/UNC Lineberger research project teams. "By being a part of this groundbreaking research I will be able to provide input and insight as an actual metastatic breast cancer patient on the design, conduct, analysis, and dissemination of the findings.”
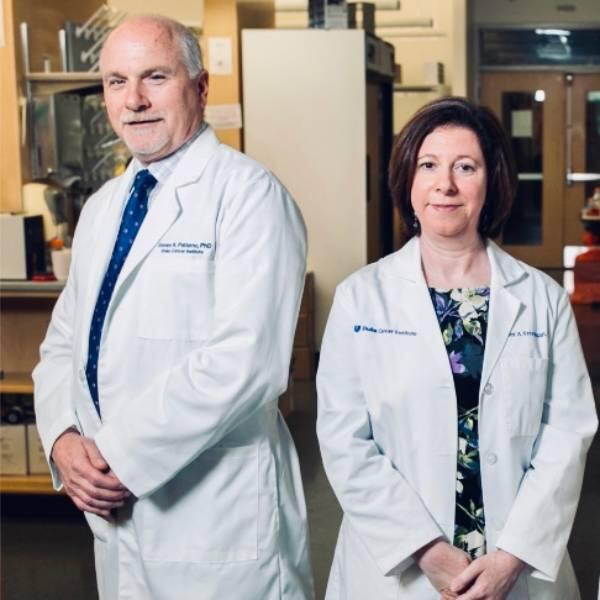
Zachary Hartman, PhD (Duke Cancer Institute) and Benjamin Vincent, MD (UNC Lineberger Comprehensive Cancer Center) are the recipients of the Susan G. Komen Metastatic Breast Cancer Collaborative Research Grant, which was supported by funds raised by individuals and organizations in North Carolina and across the country. Their research team will develop a personalized anti-tumor vaccine strategy for patients with advanced triple negative breast cancer that would mobilize the body’s immune system (primarily T cells) to shut down tumor growth and metastasis.
Ultimately, they hope to test this in Phase I proof-of-concept clinical trials at Duke and UNC in conjunction with biotech company *Replicate Bioscience, Inc., the maker of the vaccine.
“This collaboration will be essential to moving into the next phase of research — clinical trials,” said Hartman. “Patient advocates will be an active part of our team and will meet with us on a regular basis to see data and provide feedback. In the long term, they’ll be instrumental to patient engagement and advocacy in support of the Phase I clinical trial.”